Spontaneous Pneumothorax
- Primary pneumothoraces occur in otherwise healthy people without any lung disease
- Secondary pneumothoraces arise in subjects with underlying lung disease.
- Incidence up to 28/100,000 per year
- Risk of recurrence 54% in first 4 years
- No need for CXR in expiration
- CT recommended
- Differentiate pneumothorax from bullous disease
- Plain film obscured by subcutaneous emphysema
- Symptoms associated with secondary pneumothoraces are more severe
- Many patients with primary pneumnothoraces do not seek help for several days (important in re-expansion pulmonary oedema)
- Plain PA CXR underestimates pneumothorax size
- Large or small pneumothorax defined by distance between lung margin and chest wall greater or less than 2 cm (at level of hilum)
- 2cm gap = 50% pneumothorax by volume
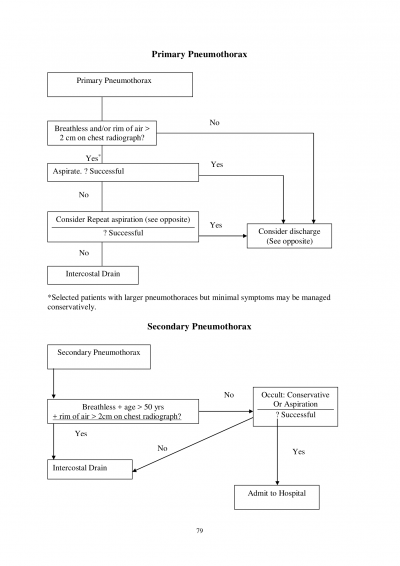
Management
- As per flow sheet opposite.
- Aspiration is first line treatment for all symptomatic primary pneumothoraces.
- If a chest drain is indicated use size 8-14 F.
- Ask senior ED doctor to supervise chest tube insertion.
- All patients with secondary pneumothoraces require hospital admission.
Aspiration
- Special kits are available which use a seldinger technique and have a non kinking catheter. Otherwise use a 14 G venflon, a three way tap and a 50 ml syringe. This can be left in until post CXR in case further aspiration is needed. - If the 1st aspiration was unsuccessful, then a second attempt at simple aspiration of the pneumothorax should be considered unless >2.5 l was aspirated during the unsuccessful first attempt.
- Repeat CXR after aspiration
Discharge
- Patients with a small (<2cm) primary pneumothorax without breathlessness should be considered for discharge with next day ED follow up for repeat CXR.
- Primary pneumothoraces that have been successfully aspirated can be discharged after a four hour period of observation
- All patients who are discharged should be reviewed within 24 hours for repeat CXR
Discharge instructions
- All patients to be advised to return if worsening breathlessness or pain
- Patients should not fly for one weeks after CXR resolution of the pneumothorax
- Should avoid exercise and using wind instruments until symptoms fully resolved
- Patients should not scuba dive unless they have a surgical pleurectomy
MacDuff A et al. Management of spontaneous pneumothorax: British Thoracic Society pleural disease guideline 2010. Thorax 2010;65 (Supp 2):ii18-ii31.