Introduction
The decision to x-ray a patient will depend on the probability of finding an abnormality based on an assessment of the mechanism of injury, the past medical history and the physical signs detected.
Have a low threshold for x-raying:
- Potentially serious injuries (e.g. cervical spine, hip).
- The very young (greenstick fractures may have minimal signs).
- The very old.
- If there is significant past history, e.g. osteogenesis imperfecta, steroid therapy, known malignancy (possibility of pathological fracture), recent injury or metal in situ.
- If there are assessment difficulties, e.g. altered consciousness, peripheral neuropathy, major learning difficulties.
- When there is a possibility of glass in a wound.
- Dog bites over hands or bony areas
Have a high threshold for x-raying if:
- The mechanism, history and examination do not suggest a bony injury.
- The presence of a fracture need not alter patient management, e.g. rib, nose or toe.
Factors which one should look for on physical examination are:
- bony tenderness (it would be unusual to have a fracture which was not tender)
- swelling or deformity
- haemarthrosis - any intra-articular fracture will cause a haemarthrosis (unless there is an associated capsular tear) and so a joint with no effusion and a full range of movement can usually be assumed not to have an intra-articular fracture.
Cervical Spine
The cervical spine must be X-rayed in all patients who have suffered a head injury or blunt trauma above the clavicles, and in whom you cannot assess the neck because of, diminished level of consciousness, alcohol etc. The cervical spine must also be X-rayed in anybody with neck pain following an injury unless they fulfil the following 5 criteria*
1. Are alert and orientated i.e. GCS 15
2. Are not intoxicated
3. Have no distracting injuries
4. Have no midline bony tenderness,
5. Have no abnormal neurology.
Alternatively, the Canadian C-spine rule can be utilised. There is no need to routinely X-ray the neck in patients with neck pain in the absence of trauma.
Other Spinal X-rays
The spine should always be X-rayed in patients with back pain following trauma when there is bony tenderness, diminished movements, or where one cannot fully assess the back because of other injuries. The whole thoracic and lumbar spine should be X-rayed routinely in all patients with multiple injuries (though this need not be done as an emergency procedure in the resuscitation room).
There is no need to routinely X-ray the lumbar spine of patients with acute back pain without trauma.
Chest
The chest must be x-rayed in:
- All patients with major trauma (even if there is no obvious chest injury).
- All patients with a chest injury caused by a high velocity injury.
- If there is a possibility of multiple rib fractures, a haemopneumothorax or visceral injury.
A chest x-ray demonstrating an isolated rib fracture will not alter management after blunt chest trauma and so it is not always necessary to x-ray a patient to exclude a rib fracture especially if several days have elapsed since the injury.
Pre-existing lung disease should lower the threshold for x-ray.
A PA erect chest x-ray is preferred. Rib views are not necessary.
Shoulder
It is important to identify the point of maximum tenderness. If you suspect an acromio-clavicular joint problem, you should request acromio-clavicular x-rays and if you suspect sterno-clavicular dislocation you should requested sterno-clavicular x-rays or a CT (ask advice). The shoulder should be x-rayed in patients who have bony tenderness or diminished shoulder movements following injury. You need two x-rays at right angles - ideally an AP and an axial. If the radiographers cannot obtain an axial x-ray they should do a trans-scapular lateral (Y view)
Elbow
Most elbow fractures are intra-articular and these will cause a haemarthrosis and diminished elbow movements especially a block to extension. The elbow should therefore be x-rayed after an injury if the patient has a diminished range of movement or if the patient has significant swelling. There is no need to x-ray children with pulled elbows.
Wrist
The wrist should be x-rayed following an injury if the patient has bony tenderness or a diminished range of wrist movement. If the tenderness is maximal in the anatomical snuff box ask for scaphoid x-rays in addition to wrist x-rays. If you are suspicious enough of a scaphoid fracture to request a scaphoid x-ray the patient must be followed up in the Review Clinic. There is no need to x-ray patients with typical tenosynovitis or with de Quervain's syndrome.
Hand
Patients should be x-rayed post-injury if there is bony tenderness or diminished range of movement of a joint. Be specific as to the site of the injury and the x-rays you request. If the patient has a finger injury you should request a finger x-ray and if the patient has a thumb injury you should request a thumb x-ray, not a hand x-ray. PIP joint injuries are easily missed on a hand x-ray. There is no need to routinely x-ray amputated finger-tips (you can look and see if there is bony involvement) or closed injuries of adult terminal phalanges where there is full active movement of the DIP joint (management will not be altered by a fractured terminal phalanx not involving the joint). There is no need to x-ray trigger fingers and trigger thumbs.
Mallet fingers should normally be x-rayed to exclude a fracture. Children with injuries of the terminal phalanx and bleeding from around the nail or displacement of the nail from the nail fold should be x-rayed to exclude epiphyseal injuries.
Lower Limb
The inability to weight-bear is almost always an indication to x-ray at least some part of the lower limb. NB the ability to weight-bear does not exclude significant injury.
Pelvis and Hip
The hip must be x-rayed in all elderly patients who fall and who complain of pain anywhere between the waist and the knee, in all elderly patients who have gone off their feet for no apparent reason and in all elderly patients with recent hip pain, or an exacerbation of long-standing hip pain, even in the absence of trauma.
In a patient with a severe injury of the lower limb it is impossible to move the leg around to exclude a hip injury and so the hip should always be x-rayed in such patients. In patients in whom the femur is injured you must ensure that you see the hip on the x-ray. The pelvis must be x-rayed routinely in all patients who have suffered major trauma. (In children aged 10 to 16 in whom you wish to exclude a slipped upper femoral epiphysis (SUFE) you should request not only an AP x-ray but a frog-leg lateral as well).
Femur
Unless the patient has a neurological deficit causing loss of sensation and paralysis of the thigh muscles, fractured femurs are usually obvious and so there is usually no indication to x-ray the femur unless there is an obvious fracture.
Knee
X-ray the knee according to the recommendations of the Ottawa knee rules. A knee X-ray series is only required for knee injury patients with any of these findings:
- Age 55 or older
- Isolated tenderness of the patella (i.e. no bony tenderness of the knee other than the patella).
- Tenderness at the head of the fibula.
- Inability to flex to 90 degrees.
- Inability to bear weight both immediately and in the ED (4 steps; unable to transfer weight twice onto each lower limb regardless of limping).
Do not routinely x-ray patients with atraumatic knee pain e.g. Osgood Schlatter's disease or chondromalacia patellae (anterior knee pain). Remember that hip problems such as slipped upper femoral epiphysis can present as knee pain.
Injuries of the Tibia and Fibula
Patients with fractures of the tibia are unlikely to be able to weight bear (beware the footballer kicked in the shin) and so patients should be x-rayed if there is bony tenderness over the tibia and an inability to weight bear. Patients with a fractured fibula may be able to weight bear and so all patients who are tender over the mid-shaft of the fibula should be x-rayed.
Ankle
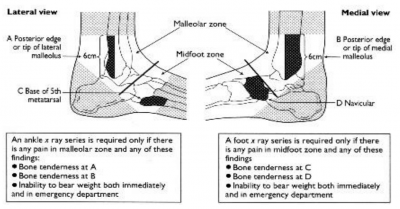
When deciding whether to X-ray the ankle or foot following an inversion injury, use the Ottawa ankle rules:
There is pain in the malleolar zone and either:
1. Bone tenderness at A or
2. Bone tenderness at B or
3. Inability to weight bear (4 consecutive steps) both immediately and in the ED
4. Age >50 or have fallen down more than 2 steps.
In ankle injuries do not ask for foot x-rays routinely.
Foot X-rays are only required if:
There is pain in the midfoot zone and either:
1. Bone tenderness at C or
2. Bone tenderness at D or
3. Inability to weight bear (4 consecutive steps) both immediately and in the ED.
In all patients with ankle injuries also palpate for tenderness over the calcaneum and the base of the 5th metatarsal. If there is calcaneal tenderness, ask for calcaneal x-rays. If there is tenderness over the 5th metatarsal or anywhere else in the forefoot ask for foot x-rays.
Foot
In all patients with severe trauma to the mid-tarsal region, ask for a true lateral x-ray of the foot in addition to the usual AP and oblique x-rays. This will avoid missing midtarsal dislocations.
Be specific about the X-rays you request: in injuries of the metatarsals and toes, ask for x-rays of the forefoot rather than the foot. For injuries of the big toe ask for an x-ray of the big toe rather than the foot or forefoot.
In general the indications for x-raying the foot are bony tenderness and an inability to weight-bear.
NB a case is sometimes made for not x-raying the injured toe as there is no specific treatment for a closed undisplaced toe fracture. This may well be so with direct trauma (e.g. a weight falling onto the toe) but a stubbed toe should be x-rayed if there is clinical evidence of a fracture as otherwise displaced fractures or dislocations may be overlooked.
Face
There is no need to x-ray the nose; if it is flattened or deviated it requires manipulation, whether or not you can see a fracture and if it is straight then it needs no treatment irrespective of whether there is a fracture.
Facial bones should be x-rayed if there is clinical evidence of a fracture i.e. a significant black eye, a subconjunctival haemorrhage without a posterior limit, bony tenderness, a step in the infra-orbital rim, deformity, tenderness over the fronto-zygomatic suture or the zygomatic arch, diplopia or infraorbital paraesthesia. NB there is no point x-raying facial bones if the patient is uncooperative or drunk as poor quality films will be taken and will need to be repeated later. Therefore, admit the patient and get further x-rays when the patient is sober or more co-operative.
Mandible
The mandible should be x-rayed (including an OPG) if there is tenderness, swelling inside or outside the mouth, or in the presence of mal-occlusion of the teeth, diminished movements at the tempero-mandibular joint or inability to bite on a tongue depressor.
Swallowed Foreign Body
If the object is of the size that might stick in the pharynx or oesophagus (e.g. a coin) or if there is any possibility that the foreign body could have been inhaled, then x-ray the neck and chest. Once a foreign body is in the stomach it will pass, and so in general terms, there is no point in x-raying the abdomen for inert swallowed foreign bodies. However, the abdomen should be x-rayed if the swallowed foreign body is a button-battery (see page 61).
Foreign Body in a Wound
If there is any possibility of there being a radio-opaque foreign body in a wound the area should be x-rayed with a marker on over the entry site. If the x-ray shows a foreign body the marker should be left on until the patient has been seen by a more senior doctor. All wounds caused by broken glass should be x-rayed.
Post reduction.
If you manipulate a fracture or a dislocation always do a post reduction x-ray.